Content
- Cardiovascular system
- Cardiovascular responses to exercise
- Vasomotor control and vascular shunt mechanisms
- Respiratory system and control mechanisms of breathing
The primary purposes of the cardiovascular and respiratory systems are to deliver adequate amounts of oxygen and remove waste from working muscles. During exercise, the reason for cardiovascular regulation is to maintain adequate blood flow in order to carry oxygen to working muscles. In addition, the circulatory system transports nutrients, e.g. glucose, and aids in temperature regulation. During exercise, the demand for oxygen to the muscles is 15 to 25 times greater than at rest. The heart cannot accomplish this by itself, and does not work in isolation. The respiratory system and cardiovascular system function together as a ‘coupled unit’, delivering the body’s oxygen and nutrients and taking away carbon dioxide and other waste to maintain homeostasis.
The cardiovascular system consists of the heart, blood vessels and blood. The blood vessels of the body responsible for carrying blood include arteries, arterioles, capillaries, venules and veins. The cardiovascular system is responsible for:
The heart is a four-chambered dual-action pump, where each side (left and right) operates separately. A muscular wall of tissue known as the septum separates the left and right sides of the heart. The right side of the heart receives deoxygenated blood from the muscles and other tissues and pumps it to the lungs for oxygenation. The left side of the heart receives oxygenated blood from the lungs and pumps it to the muscles and other tissues of the body. Each heartbeat results in the simultaneous pumping of both sides of the heart, making the heart a very efficient pump.
There are two main circulatory loops in the human body, the pulmonary loop and the systemic loop.

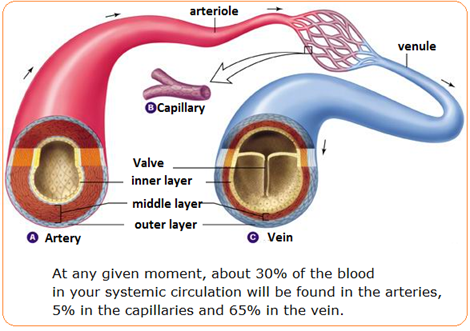
There are three major types of blood vessels: arteries, capillaries and veins. Blood vessels are the body’s highways that allow blood to flow quickly and efficiently from the heart to all parts of the body, e.g. muscles, before it returns. All blood vessels contain a hollow area called the lumen through which blood is able to flow. Around the lumen there is the wall of the vessel, which may be thin in the case of capillaries, or very thick in the case of arteries.
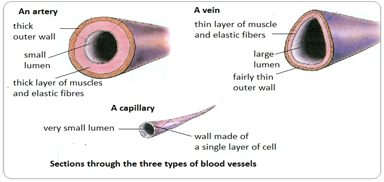
Arteries are blood vessels that carry blood away from the heart via the aorta. Blood carried by arteries is usually highly oxygenated, after leaving the lungs on its way to the body’s muscles and other tissues. The only exception to this is the pulmonary artery, which carries deoxygenated blood for the right side of the heart to the lungs before the blood becomes re-oxygenated through gaseous exchange.
Arteries face high levels of blood pressure as they carry blood being pushed from the heart under great force. To withstand this pressure, the walls of the arteries are thicker, more elastic, and more muscular than those of other vessels such as veins and venules. The largest arteries of the body contain the most elastic tissue that allows them to vasodilate and vasoconstrict and accommodate the high pressure of blood being pumped from the heart.
Arterioles are narrow vessels that branch off from the ends of arteries and carry blood to capillaries. They have much lower blood pressures than arteries due to their greater number and density and the further distance they are away from the heart. Thus, arteriole walls are much thinner than those of arteries. Nevertheless, arterioles, like arteries, have smooth muscle to control their diameter and vasodilate and vasoconstrict to regulate blood flow and blood pressure.
Capillaries are the smallest and thinnest of the blood vessels in the body. They transport the oxygen-rich red blood cells through them, allowing oxygen to diffuse into the muscles and carbon dioxide to diffuse out. The walls of capillaries consist only of a thin layer of endothelium so the movement of oxygen and carbon dioxide between the capillaries and blood is made easier.
Veins carry deoxygenated blood back to the heart and onto the lungs. Because the arteries, arterioles, and capillaries absorb most of the force and pressure of the heart’s contractions, veins and venules have very low blood pressures. This lack of pressure allows the walls of veins to be much thinner, less elastic, and less muscular than the walls of arteries.
Because of the very low pressure of the blood in the veins and venules, the body has a problem in returning blood back to the heat. There are three main mechanisms that achieve this:
Action of the muscle pump – When we move, muscle contract and relax. These contractions squeeze blood through the veins and venules. Muscle contractions help push blood back to the heart. This is a reason why we should cool down after intense exercise. By jogging, there are greater numbers of muscular contractions, which allow more blood to be returned to the heart (venous return).
Actions of respiratory pump – Similar to the muscle pump, when the diaphragm and intercostal muscles contract and relax, their rhythmic action forces blood through the veins and venules.
Pocket valves – Some veins contain many one-way valves that prevent blood from flowing away from the heart. As stated, when skeletal muscles in the body contract, they squeeze nearby veins and push blood through valves closer to the heart. When the muscle relaxes, the valve traps the blood until another contraction pushes the blood closer to the heart.
Venules are similar to arterioles as they are small vessels that connect capillaries, but unlike arterioles, venules connect to veins instead of arteries. Venules pick up blood from many capillaries and deposit it into larger veins for transport back to the heart.
The average human body contains approximately 4 to 5 litres of blood. Blood has three main functions in terms of transportation, protection and thermoregulation.
Blood is transported to almost all of the body’s tissues. The blood delivers essential nutrients (fat, protein and carbohydrate) and oxygen and removes wastes and carbon dioxide to be processed or removed from the body. Hormones (insulin) are also transported throughout the body via the blood’s liquid plasma.
The body protects itself and fights infection through its white blood cells. Platelets and red blood cells form scabs to seal wounds and prevent pathogens (infection) from entering the body and liquids from leaking out.
Temperature regulation is a key role carried out by the blood vessels and the blood. Blood vessels help maintain a stable body temperature by controlling the blood flow to the surface of the skin. Blood vessels near the skin’s surface open during times of overheating to allow hot blood to release its heat into the air (convection). We sweat when the warm air from the blood meets the cooler air temperature, the air condenses to a liquid, that liquid is the sweat we see on our skin.
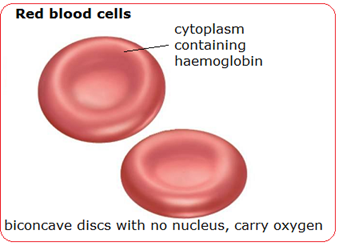
Red blood cells, also known as erythrocytes, are by far the most common type of blood cell and make up about 45% of blood volume. Erythrocytes are produced inside bone marrow at a rate of about 2 million cells every second. They transport oxygen in the blood through the red pigment haemoglobin. The shape of erythrocytes is biconcave. They are able to fold and become thinner to fit into the capillaries, the shape within the capillaries gives these cells a greater surface area to aid diffusion of oxygen.
Cardiac output mL/min = heart rate (beats/min) x stroke volume (mL)
An average person has a resting heart rate of 70 beats/minute and a resting stroke volume of 70 mL/beat. The cardiac output for this person at rest is:
Cardiac output = 72 (beats/min) x 70 (mL/beat) = 5040 mL/minute.
The total volume of blood in the circulatory system of an average person is about 5 litres (5000 mL), therefore entire volume of blood within the circulatory system is pumped by the heart each minute (at rest). During intense exercise, the cardiac output can increase up to 7 fold (35 litres/minute)
Heart rate and stroke volume increase proportionally with exercise intensity. In untrained individuals, stroke volume at rest averages 50–70ml/beat increasing up to 110–130ml/beat during intense, physical activity. In elite athletes, resting stroke volume averages 90–110ml/beat increasing to as much as 150–220ml/beat. This is achieved because the athlete has a thicker myocardium (heart muscle) on the left side of the heart. The heart is therefore able to contract with greater force, increasing the ejection fraction of blood out of the left ventricle. The ejection fraction is the amount, or percentage, of blood that is pumped (or ejected) out of the ventricles with each contraction. A normal heart pumps just over half the heart's volume of blood with each beat – an average ejection fraction is 50 to 70 percent. With prolonged training it can increase by 7–10%. Hence increased stroke volume through training, leads to an increased ejection fraction.
Stroke volume may increase only up to 40–60% of maximal capacity, after which it plateaus. Therefore, stroke volume remains unchanged right up until the point of exhaustion. The reason why we are able to continue increasing the intensity of exercise is because of the continued increase in heart rate. However, this is not conclusive since some research suggests that stroke volume continues to rise until the point of exhaustion.
An example would be: an athlete with a max heart rate of 194bpm and a stroke volume of 180mL/beat achieves a maximum cardiac output of 35L/min of blood.
180 x 195 = 35,000ml/min (35L/min)
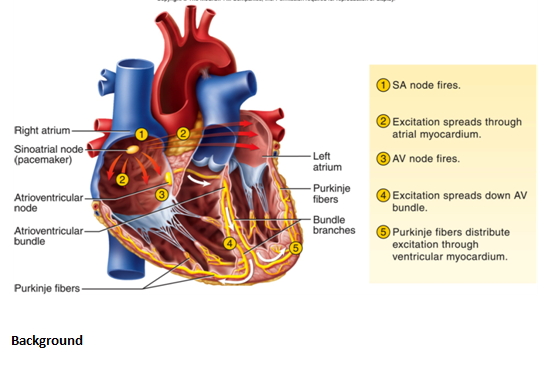
Control of heart rate is carried out in the cardiac control centre (CCC) found in the medulla oblongata of the brain; this is part of the autonomic nervous system (ANS). The (ANS) has two sub-divisions, the sympathetic nervous system (SNS), which speeds up heart rate via the cardiac accelerator nerve and the parasympathetic nervous system (PNS), which slows heart rate through the vagus nerve. Both the accelerator nerves and the vagus nerve send messages to the sino-atrial node (SA), which is responsible for controlling heart rate.
The heart has an electrical conduction system made up of two nodes they are the sino-atrial node (SA) and the atrioventricular node (AV). Unlike voluntary skeletal muscle, the heart produces its own impulses (myogenic) and hence these impulses spread throughout the heart causing the heart muscle (myocardium) to contract. A heartbeat begins with an electrical impulse from the sino atrial (SA) node. The SA node is also referred to as the pacemaker of the heart, responsible for setting rate and rhythm and is located in the wall of the right atrium. The impulse spreads through the walls of the atria (atrial systole), causing them to contract, forcing the blood into the ventricles. Then the impulse moves through the atrioventricular (AV) node (a relay station), located at the junction between the atria and ventricles. As the impulse travels down the bundle of His and onto the Purkinje fibres, the ventricles contract (ventricular systole), blood is then ejected from the heart and the cycle repeats itself. This cycle of atrial and ventricular contractions pumps blood from the heart to the rest of the body.
http://drbenzur.com/wordpress/wp-content/uploads/2014/11/svt2.png
When our bodies are at rest, the parasympathetic nervous system is in control of heart rate. The (PNS) keeps heart rate down via the vagus nerve, which releases a hormone called acetylcholine. Exercising for any duration will increase heart rate and will remain elevated for as long as the exercise is continued. At the beginning of exercise, your body removes the parasympathetic stimulation, which enables the heart rate to gradually increase. Subsequently, as exercise increases in intensity, the sympathetic nervous system becomes more dominant and takes control of heart rate. The cardiac control centre (CCC) has three ways of regulating or controlling heart rate. This refers to the mechanism that causes the heart rate to increase and decrease.
There are 3 control mechanisms of heart rate (HR):

Neural and hormonal control are considered external control mechanisms of HR, while intrinsic control is the heart’s own internal mechanism, controlling both rhythm and depth of HR.
This involves receptors picking up changes in the body as a result of increased physical activity. These then send messages to the CCC in the medulla oblongata. The ANS in the brain in turn sends a message to the SA node to either speed up or slow down the heart rate. The receptors that pick up the changes are:
Proprioceptors (Golgi tendon organs) – These pick up movement in joints and muscles. An increase in intensity of exercise generally means increased amounts of movement. The proprioceptors pick up this change and relay the information to the CCC, which increases HR and stroke volume (SV) to meet demand.
Chemoreceptors (found in muscle tissue, aorta, carotid artery) – These pick up chemical changes such as a lowering of blood pH (blood becomes more acidic). The increase in acidity (lowering of pH) occurs because as exercise intensity increases, there is an increase in carbon dioxide, which is carried in the blood as carbonic acid. Also, there is an increase in lactic acid production, so combined with the carbonic acid, the blood pH lowers. Such changes are picked up by the chemoreceptors and information is relayed to the CCC, which increases HR and SV.
Baroreceptors (found in aorta and carotid artery) – These pick up changes in blood pressure as the result of increased exercise intensity.
Thermoreceptors (found in the skin, skeletal muscle and liver) – These pick up changes in body temperature. As exercise intensity increases, then there is an increase in body temperature, which is detected by the thermoreceptors.
This involves receptors picking up changes in the body as a result of increased physical activity. These then send messages to the CCC in the medulla oblongata. The ANS in the brain in turn sends a message to the SA node to either speed up or slow down the heart rate. The receptors that pick up the changes are:
When exercise intensity begins to drop and the individual recovers, the hormone acetylcholine takes over and begins to lower HR.
This is the heart internally controlling itself. There are two factors to consider:
Temperature – As the temperature of the body tissue, e.g. cardiac muscle increases, the speed of nerve impulses speed up, which in turn increases HR.
Venous return (deoxygenated blood returning to the heart) – This is also known as Starling’s Law of the heart – As venous return increases, so does SV. Increased blood flow back into the heart causes the heart chambers to stretch, which leads to the myocardium (heart muscle) contracting with greater force, sending more blood out of the heart per beat.
After exercise, temperature and venous return decrease, which leads to both of these processes being reversed, resulting in HR and SV decreasing.
When exercise intensity begins to drop and the individual recovers, the hormone acetylcholine takes over and begins to lower HR.
Redistribution of blood flow during exercise
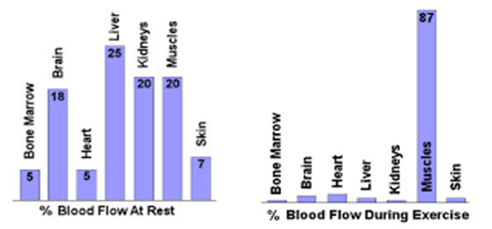
http://ibstudy.weebly.com/topic-2-exercise-physiology.html
When at rest, the muscles receive a relatively small amount of blood as they are not active. The flow of blood primarily goes to the kidneys, liver and intestine to carry out normal body functions such as digestion and removal of waste products. However, during exercise, because of the increased demand for oxygen from the muscles, the distribution of blood changes. A great deal more oxygenated blood is required by the muscles in order to produce energy (ATP) for movement. This process of increasing the blood flow to the muscles during exercise is called the vascular shunt mechanism.
This is achieved through a number of mechanisms:
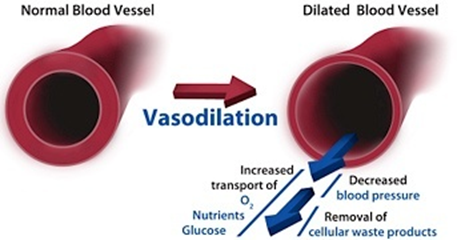
Vasodilation of arterioles – This is when arterioles going to the capillary beds of the muscles widen and increase in diameter, which in turn increases blood flow to the muscles.
Vasoconstriction of arterioles – This is the narrowing and subsequent decrease in diameter of arterioles going to the kidney, liver and intestines, reducing the blood flow to these areas.
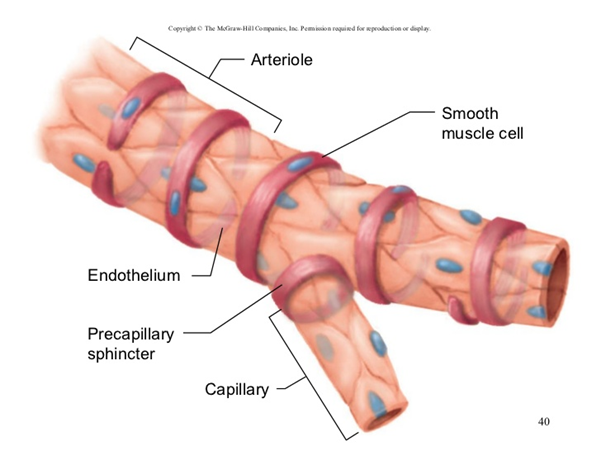
Redistribution of blood flow during exercise
Pre-capillary sphincters – These are ring-like muscles situated between the arterioles and capillaries, acting like doors that can open and close, increasing or decreasing blood flow to that area. During exercise the pre-capillary sphincters open for the capillaries feeding the muscles, and subsequently close to the kidney, liver and gut.
Redistribution of blood flow during exercise
As is the case with the control of heart rate and breathing, chemoreceptors pick up chemical changes in the blood through an increase in carbonic acid (CO2 in blood) and lactic acid. Similarly, baroreceptors pick up changes in systolic blood pressure in the aorta and carotid artery. These receptors send this information to the vascular control centre (VCC) in the medulla oblongata.
Arterioles have a middle layer of muscle which is connected to the (VCC). When this layer of muscle is stimulated via the sympathetic nerve, vasoconstriction occurs, decreasing blood flow to an area, e.g. kidneys. By decreasing the stimulation, the arteriole vasodilates, which increases blood flow, e.g. muscles. This neural control also dictates whether the pre-capillary sphincter opens or closes.
Two of the major functions of the respiratory system are to:
As with the cardiovascular system (heart, blood and blood vessels), greater demand is placed on the respiratory system as exercise intensity increases. As exercise begins, ventilation (breathing) increases in direct proportion to the intensity and metabolic energy needs of the exercise.
Ventilation increases to meet the demands of exercise through the following two methods:
If the exercise is intense, breathing rates may increase from a typical resting rate of 15 breaths per minute up to 40–50 breaths per minute.
The most commonly used measure of respiratory function is an individual’s VO2 (volume of oxygen uptake). VO2 refers to the amount of oxygen taken up and used by the body. VO2 increases linearly with increases in exercise intensity. This is due to an increasing reliance on oxygen to help provide energy as exercise continues. As the intensity of exercise continues to increase, a person reaches a maximum point above which oxygen consumption will not increase any further. This is the VO2 max. VO2 max is the maximum amount of oxygen that can be consumed and used per minute. This is often used as a measure of an individual’s aerobic fitness. The multi-stage fitness test estimates an individual’s VO2 max.
Mechanics of breathing

http://www.leavingcertbiology.net/chapter-35-the-human-breathing-system.html
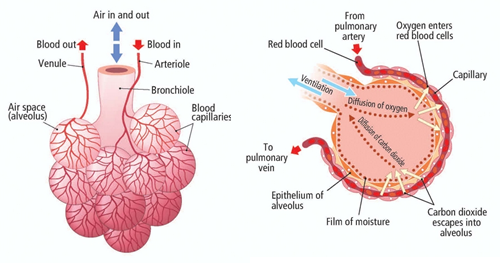
The main function of the respiratory system is gaseous exchange. This refers to the process of oxygen and carbon dioxide moving between the lungs and blood. This occurs because of the process of diffusion. Diffusion occurs when molecules move from an area of high concentration to an area of low concentration until equilibrium is reached.
Diffusion occurs during gaseous exchange as the air in the alveoli has a higher concentration of O2 than in the capillaries and therefore diffuses across into the red blood cells. Similarly, there is a greater concentration of CO2 in the capillaries than in the alveoli and therefore the CO2 diffuses across. The greater the difference in concentration between O2 and CO2 in the capillaries and alveoli, the faster the rate of diffusion (increased diffusion gradient). There is an increased rate of diffusion during intense exercise.
Both alveoli and capillaries have very thin walls, which are only one cell thick and allow gases to diffuse across them with ease.
Mechanics of breathing
http://www.leavingcertbiology.net/chapter-35-the-human-breathing-system.html
The rate of inspiration and expiration is controlled by the respiratory control centre (RCC) found within the medulla oblongata in the brain. Inspiration occurs due to increased firing of inspiratory nerves, stimulating the motor units within the intercostal and diaphragm muscles. Exhalation occurs due to a sudden stop in impulses along the inspiratory nerves. Our lungs are prevented from excess inspiration due to stretch receptors within the bronchi and bronchioles, which send impulses to the medulla oblongata when stimulated.
As with the control of heart rate, breathing rate is controlled by:
These receptors detect changes that occur during exercise and adjust breathing rates accordingly. An increase in exercise intensity causes the sympathetic nervous system to send impulses to the diaphragm and intercostal muscles, increasing breathing rate.